Putting patients in the driver’s seat
The days when patients stood back and let their health care providers make all the decisions about the treatments they received are long gone, and many believe it’s about time. After all, who better than patients themselves to be involved in the health care decisions that will affect their future — particularly when it comes to chronic respiratory conditions requiring lifestyle changes to maximize quality of life.
That was the premise behind the AARC Respiratory Patient Advocacy Summit that took place Friday afternoon. The Summit brought patients, caregivers, respiratory therapists, and others together for a unique view on the challenges and needs of patients. The Summit also addressed how patients can gain better access to clinical resources, and the role of patient advocacy groups in making this happen.
Many thanks to the Alpha One/COPD Foundation, COPD Coalition, and Allergy & Asthma Network for facilitating this important program.
School kids hear from keynote speaker
Patrick Reynolds came to Tampa this week to deliver the keynote address at AARC Congress 2015. But he also took time out of his schedule to travel to Sam Rampello Downtown Partnership K-8 Magnet School (802 E. Washington St., Tampa) with AARC leaders to talk to a group of local schoolchildren about the dangers of smoking.
It’s something this grandson of RJ Reynolds and anti-tobacco activist does whenever he goes to speak, and he believes it’s a vital part of his mission to make sure more kids never take that first puff — or if they already have, that they quit before the habit is so ingrained in their behavior that they can’t let it go.
With the rise of e-cigarettes and “vaping,” these days he is especially interested in making sure kids have the straight story about this latest threat as well, and he made that clear during his talk on Friday.
Said Reynolds before the presentation, “We have no idea how safe vaping really is, and it will be decades before we get long-term reliable data. It may be safer than smoking cigarettes, but that doesn’t mean it is safe. What I tell people in my talks is vaping may be like jumping off the fifth story instead of the tenth story.”
Cruising for a cause
The Yacht Starship pulled away from the Sail Pavilion on the south side of the convention center last night with a capacity crowd of AARC members and other dignitaries who all came on board to support the American Respiratory Care Foundation (ARCF).
The sold-out dinner cruise featured a fabulous multi-course meal, along with a short program highlighting the ARCF’s past, present, and future. Foundation donors received special recognition as well.
The highlight of the evening came with the drawing for not one, but two wonderful travel prizes: a 7-night Caribbean luxury cruise and a 3-day getaway to Las Vegas. Congrats to Karen McDonald, who won the Caribbean Cruise, and Kathy Sullivan, who will soon be headed to Vegas.
 Karen McDonald and AARC Associative Executive Director Tim Myers
Karen McDonald and AARC Associative Executive Director Tim Myers
 Kathy Sullivan and AARC Associative Executive Director Tim Myers
Kathy Sullivan and AARC Associative Executive Director Tim Myers
The Night on the Bay fundraiser was sponsored by an unrestricted grant from Vapotherm.
Congratulations, 2015 awards winners!
The following top performers in the AARC, NBRC, and CoARC received awards during this morning’s Awards Ceremony. Please join us in congratulating them on their well-deserved honors.
- Jimmy A Young Medal: Bill Galvin MSEd RRT CPFT AE-C FAARC
- NBRC/AMP William W Burgin Jr MD and Robert M Lawrence MD Education Recognition Award: Karissa L Kuneli
- William F Miller MD Postgraduate Education Recognition Award: Kelly L Colwell MRC RRT-NPS CPFT AE-C
- NBRC/AMP Gareth B Gish MS RRT Memorial Postgraduate Education Recognition Award: Kevin Collins MS RRT RPFT AE-C
- Morton B Duggan Jr Memorial Education Recognition Award: Haley Cheshier
- Jimmy A Young Memorial Education Recognition Award: Hannah R Tkach
- Charles W Serby COPD Research Fellowship: Richard D Rice MEd RRT
- Monaghan/Trudell Fellowship for Aerosol Technique Development: Allison C Anderson MSc RRT
- Philips Respironics Fellowship in Mechanical Ventilation: Dina Gomaa BS RRT
- Philips Respironics Fellowship in Non-Invasive Respiratory Care: Mark Siobal BS RRT-ACCS FAARC
- CareFusion Fellowship for Neonatal and Pediatric Therapists: Craig Smallwood BS RRT
- Forrest M Bird Lifetime Scientific Achievement Award: John B Downs MD
- Dr Charles H Hudson Award for Cardiopulmonary Public Health: William N Rom MD MPH
- Thomas L Petty MD Invacare Award for Excellence in Home Respiratory Care: Kent L Christopher MD RRT FAARC
- Mike West MBA RRT Patient Education Achievement Award: Trina M Limberg BS RRT FAARC MAACVPR
- Jeri Eiserman RRT Professional Education Research Fellowship: Robert Bayer RRT
- NBRC/AMP H Frederick Helmholz Jr MD Educational Research Grant: Monica L Schibig MA RRT-NPS CPFT
- Mallinckrodt Pharmaceuticals Best Paper Award by Best First Author: Nicholas D Werre MSRT RRT
- Draeger Literary Award: Donald A Johnston PhD RRT RN
- Albert H Andrews Jr MD Memorial Award: Paul A Selecky MD FACP FCCP FAARC
- Dr Ralph L Kendall Outstanding Site Visitor Award: Ian Gilmour MD; Kelli Chronister MS RRT-NPS CPFT
- Héctor León Garza MD Achievement Award for Excellence in International Respiratory Care: Jerome M Sullivan PhD RRT FAARC
- International Fellows: Peifeng Xu; Musa Muhtaroglu; Ramesh Unnikrishnan MSc RRT; Hussain Jassim Khatam MHS RRT FAARC
- Specialty Practitioners of the Year: Adult Acute Care, Maria Madden BS RRT-ACCS; Continuing Care/Rehabilitation, Russel Sison-Tojino RRT-NPS; Diagnostics, Matthew O’Brien MS RRT RPFT; Education, Will Beachey PhD RRT FAARC; Long Term Care, Karen Hamilton CRT; Management, Garry Kauffman MPA RRT FAARC; Neonatal-Pediatrics, Shari Toomey MBA RRT-NPS; Surface & Air Transport, Joseph Hylton BSRT RRT-NPS FCCM
- Zenith Awards: CareFusion, Philips, Fisher Paykel, Monaghan, Draeger, Aerogen
- AARC Honorary Membership: Kris Kuykendall
- AARC Life Membership: Fred Hill MA RRT-NPS
- AARC Fellows: Jeanette M Asselin MS RRT-NPS FAARC; Joseph G Sorbello MSEd RT RRT FAARC; Kenneth Miller MEd RRT-ACCS RRT-NPS AE-C FAARC; Thomas F Paolillo RRT-NPS FAARC; Diana Merendino DPT RRT-NPS RPFT FAARC; Richard Wettstein MSEd RRT FAARC; Jeffrey M Haynes RRT RPFT FAARC; John T Gallagher MPH RRT-NPS FAARC; Carolyn A Williams BS RRT FAARC; Connie Paladenech RRT RCP FAARC; John R Goodman BS RRT FAARC; Sarah M Varekojis PhD RRT RCP FAARC; Gary C White MEd RRT RPFT FAARC.
The following will be recognized in a separate awards ceremony to take place during the Annual Business Meeting tomorrow morning. Congratulations to:
- Outstanding Affiliate Contributor: Teresa Lesser RRT
- Jerry Bridgers Delegate of the Year: Chuck Menders BA RRT-ACCS AE-C
- Summit Award: South Carolina Society for Respiratory Care.
Standout companies receive Zenith Awards
 2015 Zenith Award Winners
2015 Zenith Award Winners
The AARC was pleased to bestow its annual Zenith Awards on the following companies: CareFusion, Philips, Fisher Paykel, Monaghan, Draeger, and Aerogen.
All of these companies were selected based on the quality of their products, accessibility of their sales staff, responsiveness, service record, truth in advertising, and support of the respiratory care profession.
13 members inducted into 2015 class of FAARCs
 2015 Fellows of the American Association for Respiratory Care
2015 Fellows of the American Association for Respiratory Care
Thirteen AARC members were honored as “Fellows of the American Association for Respiratory Care” during this morning’s Awards Ceremony —
- Jeanette M Asselin MS RRT-NPS FAARC
- Joseph G Sorbello MSEd RT RRT FAARC
- Kenneth Miller MEd RRT-ACCS RRT-NPS AE-C FAARC
- Thomas F Paolillo RRT-NPS FAARC
- Diana Merendino DPT RRT-NPS RPFT FAARC
- Richard Wettstein MSEd RRT FAARC
- Jeffrey M Haynes RRT RPFT FAARC
- John T Gallagher MPH RRT-NPS FAARC
- Carolyn A Williams BS RRT FAARC
- Connie Paladenech RRT RCP FAARC
- John R Goodman BS RRT FAARC
- Sarah M Varekojis PhD RRT RCP FAARC
- Gary C White MEd RRT RPFT FAARC.
All of these members have excelled in their respective areas of the profession, and we thank them for the value they have added to our field.
Jimmy A Young Medal goes to Bill Galvin
 Past AARC Executive Director Sam Giordano and Bill Galvin
Past AARC Executive Director Sam Giordano and Bill Galvin
Many of the principles that would govern our 2015 Jimmy A Young Medalist’s long career in respiratory care were developed back when he was just a teenager. “My very first job was as an orderly,” says Bill Galvin MSEd RRT CPFT AE-C FAARC. “I was probably just 16 and this taught me life lessons about caring for the ill and marginalized.”
Those early experiences with death and severe trauma stayed with him, and after earning a degree in political science from La Salle University, he focused his military service on laboratory technology. Working in the lab though just wasn’t the same as working with patients, and after he was discharged from the service, he stumbled on an advanced standing program in respiratory care at a local community college. That was all it took. He had found his calling in life.
After graduation Galvin worked as a staff therapist at Lankenau Hospital in Philadelphia, PA, where he learned the ropes from one of the pioneers in the field, George Jester. “Every day at the end of the shift George would take me into the equipment room and drill me on some pulmonary concept or piece of equipment,” he recalls. “Two hours later I would walk out thinking to myself that he is the smartest RT I ever met.”
But it was when he became assistant director of the department a few years later that his future in the profession was really set in motion. Since the manager was busy with day-to-day operations, he was assigned to handle the teaching that was needed in the department, and he loved it. “Our department taught in the nursing school, the nurse anesthetist program, the critical care course, the radiology and lab tech programs, and had clinical affiliations with local RT schools,” says Galvin. “I was the ‘go to guy’ for teaching and discovered that I really enjoyed it.”
Galvin went on to earn his master’s degree in education with a concentration in health from St Joseph’s University and transitioned into respiratory care education upon graduation, taking on the program director position at Gwynedd Mercy University. He is still there today, helping to educate the next generation of RTs.
Along the way he became actively involved in the AARC as well. A member since 1974, he first volunteered his efforts with the Pennsylvania Society and then found a role in the national organization too, working to ensure high quality continuing education programs for the AARC.
His biggest impact has probably been seen via his decades-long membership on the AARC Program Committee. Says AARC Associate Executive Director Doug Laher MBA RRT FAARC, “For the last 20 years or more Bill has, almost single-handedly, been responsible for the educational content for educators at both the Summer Forum and AARC Congress. To have that much longevity in one area of expertise is incredible.”
He’s been an active participant on the editorial front as well, publishing in professional magazines and journals and serving as a reviewer for a wide range of publications. He is also co-author, along with Dean Hess PhD RRT FAARC of a leading textbook in the profession, “Respiratory Care: Principles and Practice,” recently released in its third edition.
Read more about Bill Galvin and his contributions to respiratory care and the AARC in your September issue of AARC Times.
From tobacco company heir to anti-tobacco activist
 Patrick Reynolds
Patrick Reynolds
When Patrick Reynolds took the stage to deliver the keynote address, attendees were on the edge of their seats. Why would a man born into a family famous for its tobacco products leave it all behind to support the anti-tobacco movement?
The grandson of RJ Reynolds shared his motivations and more in a presentation that ranged from his experiences at the bedside of a father dying of emphysema to the foundation he started to make sure more people would be able to quit smoking and fewer kids would ever take up the habit.
Attendees rush in!
 Exhibit Hall Ribbon Cutting Ceremony
Exhibit Hall Ribbon Cutting Ceremony
The AARC Exhibit Hall opened up right after the Opening Ceremonies this morning and attendees lost no time getting into the hall to see the latest and greatest in respiratory care.
With all the vendors in the industry on hand, it’s a great place to see the technology that will define the profession in 2016 and beyond, and it’s a Buying Show as well. In some cases, attendees will be able to cover the cost of their trip to Tampa through the savings realized via meeting discounts.
When Sleep Testing Gets Tricky
Obstructive sleep apnea and other sleep problems are often accompanied by comorbidities that can significantly complicate testing and diagnosis. Peter Allen, BSRC, RRT-NPS, RST, RPSGT, addressed several common scenarios encountered by sleep professionals charged with testing patients with cardiovascular and associated co-morbidity issues in a talk this afternoon.
“Complex patients – that’s what we’re seeing in sleep labs today,” said the clinical coordinator and physician liaison at the Riddle and Exton Sleep Disorders Centers at Main Line Health Systems in Pennsylvania. “Comorbidities won’t bring the plane down, but you need to take care of them.”
For example, research suggests 76% of people with congestive heart failure may have OSA and 77% of those with obesity are affected.
Allen specifically covered the special considerations that must be taken when testing patients who also suffer from COPD, diabetes, morbid obesity, cardiovascular disease, congestive heart failure, and metabolic syndrome, focusing in on the need to understand which medications these individuals are taking, intake concerns that may arise when someone is referred for testing, and problems that could come up on the night of the test.
“Many people coming to the outpatient lab think they are going to get inpatient services,” he said. “So how you handle the intake makes a difference.”
For example, COPD patients who are on home oxygen will require special handling, and frequent urination is common during the polysomnography itself among those on diuretics. People who are morbidly obese may require special beds that can handle their weight, and cardiovascular patients may have a pacemaker that will have to be taken into consideration.
“If you see a medication and you don’t know what it is, ask the patient,” advised the manager. He also emphasized the need for patients to stay on their usual medication schedule. “Do not let patients take a night off.”
Allen went on to address the specific characteristics sleep professionals can expect to see in patients whose conditions overlap with OSA, such as more nocturnal desaturations in people with COPD, fluid retention in those with morbid obesity, and the Cheyne Stokes Pattern in those with heart failure.
Patients who have previously suffered a heart attack may have insomnia as well – particularly if their heart attack came during the night. Allen recalled the case of one patient who had experienced more than one heart attack at night. “He woke up every five minutes calling for his wife. It’s a scary thing, and you can have some fear coming into play.”
Allen cited a number of referral sources for these patients and how sleep centers can work with them to ensure more patients receive the testing they need to get a better night’s sleep. “Most of our referrals come from family practices,” said the manager, “but cardiologists are getting more involved.”
The good news, said Allen, is that in many cases treatment for OSA can lead to better outcomes for patients with these conditions, including decreased hospitalizations and lower readmission rates. “You will be seeing more complex cardiovascular patients,” he told his audience. “RTs are the go-to technologists for the complex patient.”
Here’s How to Hire Engaged RTs
RT managers want engaged employees for their staff, but finding them is often an uphill battle.
In this afternoon’s lecture on “Shaking the Engagement Tree – Hiring Engaged RTs,” Garry Kauffman, MPA, RRT, FAARC, FACHE shared a number of tips aimed at helping managers find the kind of staff members they need to build a successful department.
It starts by getting out there and letting the rest of the RT world see what kind of manager you are and what kind of department you run, said the management consultant. “Advertising doesn’t necessarily mean an ad in the paper,” said Kauffman. “Part of advertising is visibility.
How can you become more visible? There are a plethora of ways to do it, continued Kauffman – lecture at your state society meeting, take part in RT-related community service, volunteer to speak at your local RT school, offer a student internship, publish in RT or lung health related publications, or just get more actively involved in your AARConnect communities.
He especially advocates for the latter. “It’s one heck of a great education, and guess who’s looking at this as well? Prospective employees.”
Then, when it does come time to fill a slot, make your objectives clear in your employment ad. That two line ad seeking a 12 hour night shift RT will get you someone who’s just looking for a job. A multi-line ad spelling out your need for a critical thinking therapist who is a great team player and wants to make a real difference in the lives of his or her patients is more likely to attract someone looking for a career.
You can harness the power of your current staff as well. “The staff that I worked with knew far more than I did,” said Kauffman. “It’s better to give your applicants the real story than to sugarcoat it.”
When it’s time to interview the candidates, he recommended the behavioral interviewing route. Questions like “Tell me about your latest mistake,” “How do you deal with conflict with a co-worker,” and “Did you ever work with a slacker,” drill down into a person’s character and can help you predict how he or she will perform on the job.
One question he always found especially useful was, “What do you need in a boss?” Most often he would be met with blank stares, but getting a great answer to that question could seal the deal for a prospective employee. “It was the last discriminator I used to decide between two candidates.”
A number of new screening tools are also available to assess personality factors that tend to suggest a job candidate will go one way or the other when it comes to being engaged and Kauffman went over what’s available there as well.
Kauffman ended his talk by emphasizing the need for managers to lavish some extra attention on their new hire as well – anything from sending a “We can’t wait!” letter with a picture of staff to meeting and greeting the person on the sidewalk and walking him or her up to the department.
Then, as a part of the employee orientation process, take the time to learn a little something about the individual and his or her likes and dislikes off the job too. A short survey asking about day of birth, favorite colors, movies, musical performers, and other fun topics lets your new employee know you value him or her as more than just an RT.
Kauffman said his staff always loved knowing they’d get a blue bag with a diet Pepsi and maybe an inexpensive DVD of their favorite movie on their birthday.
Precious Cargo: The RT’s Role on Specialty Care Transport Teams
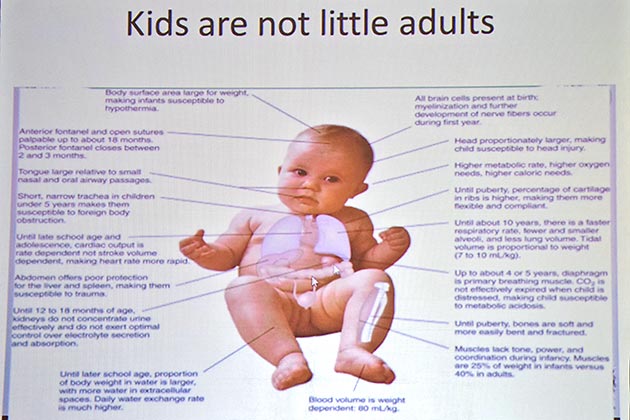
As any pediatric care provider will tell you, infants and children are not just little adults, and when they are so ill they require transport to a higher level of care, specialized transport teams step in to ensure a timely and smooth transition.
In a presentation earlier this afternoon, Alex Brendel, MBA, RRT-NPS, described the current model of transport for neonatal/pediatric patients, discussed the RT’s role on these teams, and covered the results of a survey he conducted with fellow AARC member Tabatha Dragonberry, BSRT, RRT-NPS, to learn more about how therapists are used on transport.
According to Brendel, who serves as the respiratory therapist clinical team leader of the Neo-Peds Critical Care Transport Team at the Carilion Clinic Children’s Hospital in Roanoke, VA, specialty care teams (SCTs) grew out of the need of community hospitals to deliver critically ill patients to a higher level of care.
“A large portion of medical care for children is done at community hospitals,” he said. “Children requiring transport have a higher risk of a transport-related ‘never event’ and it’s easier to avoid these if you are with a specialty care team.”
The SCT assesses the patient upon arrival, implements care according to the tertiary care facility’s clinical practices, then turns care over to hospital staff on arrival back to the tertiary care facility.
Challenges with this model range from reimbursement to ensuring enough vehicles are available to covering incidences when the primary team is out on call and another call comes in.
Team members bring a wealth of knowledge to the job, said Brendel, including expertise in assessment, goal directed therapies, resuscitation, evidence-based practice and protocols, and a solid foundation of certifications and credentials.
How do RTs figure into these teams? In the survey he conducted with Dragonberry, Brendel found RTs were significantly more likely to be used on neonatal/pediatric transport teams than adult only teams, 43% vs. 11%. But 28% of respondents said they used RTs on all three teams – neonatal, pediatric, and adult.
The RN/RT crew configuration was the most popular, at 43%, with another 12% reporting an RN/paramedic/RT configuration, 12% reporting an RN/NP or PA/RT configuration, and 6% reporting an RN/physician/RT configuration. Others said they use an RT as needed, citing escalation of care for any neonate, trach patients, and any pediatric patient with airway or pulmonary compromise as among the reasons.
RTs on these teams were found to perform a range of procedures, with ventilator management being the most common at 100% and intubation coming in second at 79%. Ninety-three percent of the respondents said their RTs are not required to have either an EMT or paramedic credential.
Not surprisingly, 98% of respondents said they used medical air and oxygen on transport, but 74% said they also used nitric oxide and 27% reported using heliox. Most of the respondents – 83% -- reported not doing scene responses and the 11% that did said they did not take RTs.
Brendel believes the survey is proof that “there are respiratory therapists out there doing lots of things” on transport, but the bottom line is RTs are still being removed from some teams to save on costs.
While levels of care being created by the Commission on Accreditation of Medical Transport Systems may help facilities determine which patients should be transported by whom, and the AARC is actively involved in education and advocacy for RTs on transport as well, clearly more research is needed to show the value therapists add to these teams.
“Your job might be on the line if we can’t prove our value,” concluded Brendel.
