Wednesday, December 8
8:30 am – 9:20 am
26th Phil Kittredge Memorial Lecture
This lecture provides a critical and incisive evaluation of an aspect of clinical respiratory care of emerging or increasing importance.
COPD Heterogeneity: What This Will Mean in Practice
Stephen I Rennard MD, Omaha NE
Dr. Rennard is Larson Professor of Medicine in the Pulmonary and Critical Care Medicine Section of the Department of Internal Medicine at the University of Nebraska Medical Center. Dr. Rennard maintains an active program of clinical investigation in COPD and tobacco-dependence treatment and a program of basic research in the mechanisms of lung tissue repair and remodeling, including the role of stem cells in disease pathogenesis and repair.
 Sputum Bowl Contestants
Sputum Bowl Contestants 9:30 am – 10:05 am
The Legacy of the ARDSnet
Jesus Villar MD PhD, Canary Islands Spain
It has been 11 years since the ARDSnetwork was published. Dr. Villar will examine where we’ve been, where we are now, and where we need to go in this controversial but vital part of our practice.
9:30 am – 10:10 am
2011: The Year in Preview
Supported by an unrestricted educational grant from
![]()
Bruce K Rubin MD MEngr MBA FAARC, Richmond VA
Dr. Rubin will speculate (based on where he thinks the field will be going) about important papers that will be published in 2011 and how these affect the practice of respiratory care.
9:30 am – 10:10 am
Novel Approaches to Improving Outcomes in Pulmonary Rehabilitation
Michele L McCarroll PhD FAACVPR, Akron OH
Pulmonary rehabilitation (PR) has been shown to improve exercise capacity and overall quality of life for patients suffering from chronic pulmonary disease; however, there is little research that demonstrates that the improvements observed in functional capacity transfers to improvements in specific activities of daily living (ADL) skills. Furthermore, it is difficult to find an ADL assessment specific to the chronic pulmonary disease population or for outpatient PR programs. Since the main objective of PR is to not only improve exercise capacity but to also improve functional independence at home, a functional activity training program may be an essential part of a successful PR program.
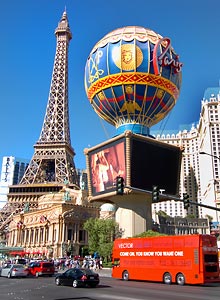 Paris Las Vegas
Paris Las Vegas
9:30 am – 10:15 am
The Upper Airway and Cardiopulmonary Exercise Testing
Carl D Mottram RRT RPFT FAARC, Rochester MN
This presentation will describe utilizing flow volume loop testing and video laryngoscopy during cardiopulmonary exercise to define flow limitations, inappropriate breathing strategies and structural upper airway abnormalities that appear during exercise sessions. Testing techniques and case studies will be reviewed.
9:30 am – 10:35 am
Unconventional and Extreme Respiratory Support
9:30 am – 10:00 am
Therapy for Patients with Refractory Hypoxemia
Randal S Blank MD PhD, Charlottesville VA
This presentation is a review of techniques for the treatment of refractory hypoxemia. After attending this lecture the therapist will be able to describe the role of pharmacologic therapies for acute pulmonary hypertension in patients with refractory hypoxemia. Surgical approaches for refractory hypoxemia including closure of right-to-left atrial shunts and extracorporeal therapies for hypoxemic respiratory failure will be discussed.
10:05 am – 10:35 am
Therapy for Extreme Hypercarbia
Charles G Durbin Jr. MD FAARC, Charlottesville VA
This presentation will describe conventional treatment approaches for patients with extreme hypercarbia and explain experimental therapies directed at controlling CO2 production while increasing its removal. The presenter will review efficacy data associated with these treatments and approaches.
 Cabo Wabo at Planet Hollywood
Cabo Wabo at Planet Hollywood
9:30 am – 11:10 am
Oxygen Therapy for Chronic Hypoxemia: What We Should Know
9:30 am – 10:00 am
State of the Art in LTOT: What Does the Science Say?
Brian W Carlin MD FAARC, Pittsburgh PA
This presentation will review current science behind the use of supplemental oxygen therapy and discuss the perceived gaps in the science and how to resolve the potential impact.
10:05 am – 10:35 am
Continuous Flow vs. Pulse Dose Delivery: Is One Better Than the Other?
Patrick J Dunne MEd RRT FAARC, Fullerton CA
This presentation will review the available data comparing the effectiveness of continuous flow to pulse dose delivery systems and will provide guidelines for the proper use of each system.
10:40 am – 11:10 am
Newer Devices for the Delivery of LTOT
Timothy W Buckley RRT FAARC, Chicago IL
This presentation will describe the newest types of oxygen delivery technologies and the advantages they portend for oxygen-dependent patients and will identify the potential limitations of certain devices for selected patient populations.
 Holiday Decorations at Bellagio
Holiday Decorations at Bellagio
9:30 am – 11:10 am
Creating and Maintaining a Culture of Safety
9:30 am – 10:00 am
Errors and the RT: Some Inconvenient Truths
John W Salyer RRT-NPS MBA, Seattle WA
The presenter will discuss cases in which RTs had a role in clinical errors, the risks associated with litigation, and how we can achieve risk reduction through improvement in clinical documentation.
10:05 am – 10:35 am
Creating a Culture of Safety in Your RC Department
Dave Crotwell RRT-NPS, Seattle WA
The presenter will address error proofing, classification of procedures, standard work, risk-benefit assessment, and using electronic incident reporting—all as a cohesive means to create a culture of safety within the RT staff.
10:40 am – 11:10 am
Back to the Bench: A Scientific Approach to Evaluating Equipment Performance and Safety in Your Department
Robert M DiBlasi RRT-NPS, Seattle WA
The presenter will address developing research questions based upon clinical reports from the bedside, designing bench studies to answer questions related to equipment performance, designing bench studies to answer questions related to patient/equipment interactions, and taking these improvements back to the bedside.
 Open Forum
Open Forum
9:30 am – 11:25 am
OPEN FORUMs #9—Management, Part 2
OPEN FORUMs #10—Aerosols/Drugs
Clinicians present the results of their scientific studies. Abstracts with a similar focus are clustered into a symposium to encourage discussions and interactions among investigators and observers; posters expand the information presented. See abstract titles and authors.
9:30 am – 11:45 am
Hot Topics in Neonatology
9:30 am – 10:00 am
Respiratory Management of the Premature Infant
Sherry L Courtney MD, Manchester NY
For the premature infant, every mechanical ventilator breath damages alveoli. What are the current strategies to reduce the incidence of chronic lung disease? What does the future hold? This presentation will answer these and other clinically relevant questions.
10:05 am – 10:35 am
The New BPD: What Does the Future Hold?
David Durand MD, Oakland CA
How has bronchopulmonary dysplasia (BPD) changed? Why have these changes occurred? What is the anticipated prognosis for premature infants born today? These and other important questions about the “New BPD” will be answered.
10:40 am – 11:10 am
Therapy for Pulmonary Hypertension: Nitric Oxide and Beyond
David Durand MD
The field of pulmonary hypertension is changing as rapidly as any other in the neonatal and pediatric worlds. New acute and chronic medications are quickly becoming available to treat this vulnerable population. One of the world’s leaders on pulmonary hypertension will review current management strategies and offer thoughtful insight into the future.
11:15 am – 11:45 am
Pulse Oximetry—Is Closed Loop Really Necessary?
Sherry E Courtney MD, New Hyde Park NY
Closed-loop FiO2 control for our ventilators is on the horizon. Many resources have been used to develop this technology. But is it really necessary? Will patient care be improved by closed-loop controls? Come hear one of the experts review the available data as well as offer speculations for the future.
 Bobby Flay’s Mesa Grill at Caesars
Bobby Flay’s Mesa Grill at Caesars
9:30 am – 12:00 noon
Controversies in the Mechanical Ventilation of Adults with Acute Respiratory Distress Syndrome
9:30 am – 9:40 am
Introduction and Explanation of Ground Rules for Pro-Con
David J Pierson MD FAARC, Seattle WA
Despite studies establishing the value of lung-protective ventilation in managing patients with ALI-ARDS, controversy persists about the “best” way to achieve this while supporting oxygenation. Although the target delivered tidal volume and optimal static airway pressure are less contentious issues than in the past, there are still numerous options in providing ventilatory support, with conflicting evidence and strongly held opinions on the part of many clinicians. This symposium highlights several of these areas of conflict, with each side of the controversy presented by a noted authority in the field.
9:45 am – 10:15 am
Airway Pressure Release Ventilation Has Important Advantages Over Conventional Volume-Targeted Ventilation for Managing ALI-ARDS
Pro: Richard D Branson MSc RRT FAARC, Cincinnati OH
Con: Neil R MacIntyre MD FAARC, Durham NC
Airway pressure release ventilation limits peak airway pressure while increasing mean airway pressure and maintaining alveoli in a maximally recruited state through prolongation of what is effectively the inspiratory phase. It also permits spontaneous breathing. The discussants review the theoretical and practical aspects of using APRV in ALI-ARDS — both pro and con — in comparison with conventional volume-targeted ventilation.
10:20 am – 10:50 am
Higher PEEP Is Better in Managing ALI-ARDS
Pro: Jesus Villar MD PhD, Canary Islands Spain
Con: Richard H Kallet MS RRT FAARC, San Francisco, CA
In the ventilatory management of patients with ALI-ARDS, higher levels of PEEP are associated with better oxygenation as measured by arterial PO2 and PaO2/FIO2 ratio. Whether this benefit is sufficient to offset the increased risks for lung over distension and hemodynamic compromise remains controversial. The discussants review the theoretical basis for higher PEEP levels and the existing evidence base in terms of both physiologic benefit and effects on patient-relevant outcomes in an attempt to clarify this contentious issue.
10:55 am – 11:25 am
PEEP Should Be Set Using Esophageal Pressure Measurements in Managing ALI-ARDS
Pro: Michael A Gentile RRT FAARC, Durham NC
Con: Carl R Hinkson RT RRT, Seattle WA
PEEP and end-inspiratory plateau pressure do not have the same implications for both benefit and harm in all patients with ALI-ARDS, and this is especially true when chest wall stiffness may be playing a role. This discussion summarizes the rationale for measuring trans-pulmonary pressure by means of an esophageal balloon and using this measurement to set PEEP. The participants will also place this newly popular procedure in clinical perspective and attempt to decide whether it is valid, safe, and clinically beneficial.
11:30 am – 12:00 noon
High-Frequency Oscillatory Ventilation Should Be Part of Your Institution’s Armamentarium for Managing Server ALI-ARDS
Pro: Neil R MacIntyre MD FAARC
Con: Dean R Hess PhD RRT FAARC, Boston MA
Some patients with severe ARDS experience critical hypoxemia despite optimal adjustment of conventional volume-targeted or pressure-targeted ventilation. HFOV is one option for managing these and other patients with hypoxemic respiratory failure. The discussants will present the advantages and disadvantages of this alternative approach to ventilatory support, from both theoretical and practical perspectives.
 Adventuredome at Circus Circus
Adventuredome at Circus Circus
10:15 am – 10:55 am
Don’t Lose Sleep Over Home Testing
Rebecca F Olson RRT, Waukesha WI
Many challenges discourage patients from testing in attended sleep labs. As a result, many do not get tested, diagnosed or treated for obstructive sleep apnea (OSA). Alternative diagnostic options for the OSA population will be explored, and the advantages and disadvantages of each methodology will be discussed, including legal aspects of home testing and self referral.
10:15 am – 11:15 am
Delivering Respiratory Care Education Via Alternative Course Delivery Methods
Shawna L Strickland PhD MEd RRT-NPS AE-C, Columbia MO
This presentation will address the use of various alternative course formats in the context of delivering respiratory care education. The presenter will provide an overview of the meaning of success in a respiratory care educational program and progress into the definition of 3 course delivery methods (traditional classroom environments, online course environments and blended learning environments). Following the establishment of baseline knowledge, the presenter will compare and contrast the various course delivery methods and identify ways to integrate these methods to facilitate maximum learning in the respiratory care educational program.
10:20 am – 11:00 am
Mobile Spirometry Unit and Its Impact on COPD Detection
Steve Nelson MS RRT FAARC, Irving TX
AARC has partnered with the COPD Foundation to do pulmonary function testing at public events since 2006. The MSU provided testing and information to more than 35,000 people with over 250 respiratory therapists participating around the country. In 2008, they began validating a method of COPD case finding from an NHLBI and COPDF consensus conference. Risk factors and PEF are used initially, instead of spirometry, to determine who would benefit from additional testing. Using PEF as the primary measure increased the number of people who had contact with respiratory therapists, while improving on the accuracy of typical public events.
 Atomic Testing Museum
Atomic Testing Museum
10:40 am – 12:20 pm
Hyperbaric Medicine
10:40 am – 11:10 am
Introduction to Hyperbaric Medicine
Clifford E Boehm MD RRT Master SCUBA Diver, Baltimore MD
This presentation will allow therapists to recognize and understand the theory of hyperbaric medicine and the approved indications for its use. Contraindications to the therapy will also be discussed.
11:15 am – 11:45 am
Hyperbaric Therapy and the Respiratory Therapist—A Perfect Fit
William C Gearhart CHT DMT EMT CFPS, Baltimore MD
This presentation will allow therapists to recognize and understand the basic fundamentals of HBOT delivery. Existing safety standards related to HBOT delivery will also be discussed.
11:50 pm – 12:20 pm
Hyperbaric Oxygen Services—This Ain’t Your Daddy’s HBO
Garry W Kauffman MPA FACHE RRT FAARC, Lancaster PA
This presentation will allow therapists to recognize and understand how to analyze HBO as a clinical service and business opportunity to enhance organizational performance. Business delivery models (in-house, out-source, collaboration) will be presented. The discussion will include an appreciation of physician demands and responsibilities related to HBO therapy.
 The Venetian Las Vegas
The Venetian Las Vegas
11:00 am – 11:30 am
Reimbursement Issues in Home Sleep Testing
Jackie McClure RRT FAARC, Melbourne Beach FL
This presentation will be a brief overview of Medicare, Medicaid and private insurance billing issues associated with home sleep testing. Reimbursement for home sleep testing as well as legal aspects of home testing will be explored.
11:05 am – 11:45 am
Diagnostics Section Membership Meeting
Michael Tracy RRT-NPS RPFT/Presiding
Section members meet to determine their needs and priorities, as well as how to use the AARC resources to accomplish them. All Congress attendees, including section non-members are invited to attend and to participate.
11:15 am – 11:55 am
Do No Harm: Cultivating a Culture of Safety and Accountability
Richard M Ford RRT FAARC, San Diego CA
Some would say that there is no more dangerous place to be on this nation than in a hospital. This presentation will define the extent of preventable deaths and injuries to patient, the cost of such failures, and how we can develop and hard-wire a culture of safety and accountability.
11:15 am – 12:00 noon
Adult Acute Care Section Membership Meeting
Michael J Hewitt RRT-NPS FAARC/Presiding
Section members meet to determine their needs and priorities, as well as how to use the AARC resources to accomplish them. All Congress attendees, including section non-members are invited to attend and to participate.
11:15 am – 12:00 noon
Home Care Section Membership Meeting
Robert W McCoy RRT FAARC/Presiding
Section members meet to determine their needs and priorities, as well as how to use the AARC resources to accomplish them. All Congress attendees, including section non-members are invited to attend and to participate.
11:25 am – 12:00
Neonatal/Pediatrics Section Membership Meeting
Brian K Walsh MBA RRT FAARC/Presiding
Section members meet to determine their needs and priorities, as well as how to use the AARC resources to accomplish them. All Congress attendees, including section non-members are invited to attend and to participate. Open Forum
Open Forum
12:30 pm – 2:55 pm
OPEN FORUMs #11—Ventilators/Ventilation, Part 1
Clinicians present the results of their scientific studies. Abstracts with a similar focus are clustered into a symposium to encourage discussions and interactions among investigators and observers; posters expand the information presented. See abstract titles and authors.
1:00 pm – 2:05 pm
Year in Review: Part 2
Supported by an unrestricted educational grant from
![]()
1:00 pm – 1:30 pm
Asthma
Bruce K Rubin MD MEngr MBA FAARC, Richmond VA
This presentation will review the most important papers published on asthma in the past year.
1:35 pm – 2:05 pm
COPD
Rajiv Dhand MD, Columbia MO
This presentation will review the most important papers published on COPD in the past year.
1:00 pm – 2:25 pm
Patient Safety: It’s Everyone’s Job!
1:00 pm – 1:40 pm
Safety Monitoring of Patients Outside of the Critical Care Environment—Implications for the Respiratory Therapist
John Sabo MS RRT RN, Houston TX
Increasing concern about patient safety in hospitals is driving new ways of thinking about patient monitoring. As more patients are being diagnosed with obstructive sleep apnea and other conditions altering responses to the pain medications, the need for novel “remote” respiratory monitoring strategies increase. The monitoring sites extend beyond critical care as patients are released to general floor care areas under opiod-based patient control anesthesia (PCA) for pain management. Surveillance monitoring of at-risk patients outside of critical care will be reviewed, and early intervention strategies for pending respiratory distress will be discussed. The difficulty in monitoring ventilation, including those using CPAP, will be discussed. Potential solutions including remote monitoring and clinician alert/notification systems will be considered.
 The Wine Tower at Aureole, Mandalay Bay
The Wine Tower at Aureole, Mandalay Bay
1:00 pm – 2:25 pm
Our Very Smallest of Patients…
1:00 pm – 1:25 pm
Ventilation Strategies for Very Low Birthweight Infants
John S Emberger RRT, Newark DE
Strategies for conventional pressure-controlled and volume-targeted ventilation for extremely low birthweight premature infants will be reviewed along with the available medical literature. Guidelines for initiating and ventilating this vulnerable population of infants will be discussed.
1:30 pm – 1:55 pm
Non-invasive Monitoring in Neonates: Can We Stop the Progression of Multi-faceted Injury in the Extremely Premature Infant?
Kathleen M Deakins RRT-NPS, Cleveland OH
As important as the advances in the ventilation of the premature infant is the non-invasive monitoring of these strategies. New techniques and strategies for the monitoring of this vulnerable population will be discussed along with the potential benefits in pulmonary and neurologic outcomes.
2:00 pm – 2:25 pm
The Changing Physical Environment: Effects on Respiratory Care
Kathleen M Deakins RRT-NPS
Does the physical environment of the NICU really matter? What are the effects of single patient rooms on the delivery of health care from patient and staff perspectives? Have family accommodations in the neonatal ICU setting interfered with the daily operations of the unit? These controversial issues and others will be discussed.
1:00 pm – 2:35 pm
Ethics and the RT
1:00 pm – 1:45 pm
Ethics: The Good, the Bad, and the Ugly
Shawna L Strickland PhD MEd RRT-NPS AE-C, Columbia MO
This presentation will address the ethical issues associated with using non-invasive ventilation to sustain life in futile situations. A review of the technology and the basic ethical principles based on the Georgetown Model will begin the session. This presenter will address situations in which the patient has completed a “do not attempt resuscitation” or “do not intubate” order, as well as situations in which the respiratory care practitioner faces ethical dilemmas as he or she strives to provide the most ethical patient care. Case scenarios will be used to stimulate thought and discourse among the audience.
1:50 pm – 2:35 pm
Respiratory Therapist as a Member of the Biomedical Ethics Committee
Douglas E Masini EdD RPFT RRT-NPS AE-C FAARC, Savannah GA
Respiratory therapists are the 911 of health care. Therefore, respiratory therapists are the best resource to communicate critical care, ventilation, and life support technology within the framework of an ethics committee. The speaker explores the emerging role of a respiratory therapist within the committee and in multidisciplinary bedside ethics consultation teams.
 Holiday Decorations on Fremont Street
Holiday Decorations on Fremont Street
1:00 pm – 3:10 pm
Above the Clouds and Under the Sea
1:00 pm – 1:40 pm
Update on Altitude-Related Illness
Andrew M Luks MD, Seattle WA
This lecture reviews that pathophysiology, clinical features, diagnostic criteria, management, and prevention of illness that develops in people who ascend to high altitude: acute mountain sickness, high-altitude pulmonary edema, high-altitude cerebral edema, and chronic mountain sickness.
1:45 pm – 2:25 pm
High-Altitude Simulation Testing
Matthew J O’Brien RRT RPFT, Madison WI
This presentation discusses the pre-travel, low-altitude evaluation of patients with cardiorespiratory disease who are at risk for development of hypoxemia when they travel to higher altitudes, via commercial airliner and by other means. After a review of the evidence base supporting the use of the High Altitude Simulation Test (HAST) and of the indications for its use, practical guidance for performing it will be presented, including equipment, gas delivery, safety, and billing and documentation.
2:30 pm – 3:10 pm
Physiology and Complications of Diving
Andrew M Luks MD
Both free diving and scuba diving can have serious respiratory-related complications. This presentation reviews the physiologic effects of both forms of diving and reviews the adverse effects that may occur, including decompression sickness and barotraumas. It includes descriptions of the clinical manifestations and management of each complication, along with methods of prevention.
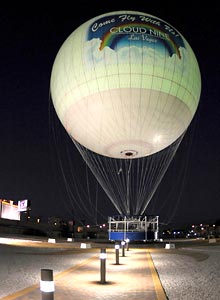 Cloud Nine Balloon Rides
Cloud Nine Balloon Rides
1:00 pm – 3:10 pm
Presentation, Assessment and Treatment of Neurologic Emergencies in the Neonatal and Pediatric Transport Setting
1:00 pm – 1:45 pm
Presentation and Assessment of Neurologic Emergencies in Infants and Children
Steven E Sittig RRT-NPS FAARC, Rochester MN
Children with neurologic diagnoses make up a large percent of patients referred for interfaculty transport. Early identification and rapid management of physiologic compromise limits the potential for secondary insults and improves outcomes. The lecture will discuss the epidemiology, assessment, and presentation of infants and children with neurologic emergencies. A review of the physiologic basisbases of the physical findings from seizures to increased intracranial pressure will be discussed. The lecture will conclude with a symptom-based approach assessment of the neurologically comprised patients.
1:50 pm – 2:35 pm
Treatment and Outcomes of Neurologic Emergencies in the Transport Setting
Bradley A Kuch RRT-NPS, Pittsburgh PA
It has been reported that under-treatment and secondary insults are major factors associated with poor outcomes in children with neurologic emergencies. The lecture will examine the most recent guidelines for the treatment of infants and children with brain injury. The evidence surrounding hypertonic (3%) saline, mannitol, and hypothermia will be reviewed. Additionally, the feasibility of controlled hypothermia in the transport setting will be discussed. The presentation will conclude with an evidence-based review of the literature surrounding the outcomes of children with neurological diagnoses.
2:40 pm – 3:10 pm
Neurologic Case Studies: When a Seizure Is Not Just Another Seizure!
Steven E Sittig RRT-NPS FAARC
Bradley A Kuch RRT-NPS
Presenters will provide an assortment of neurologic case scenarios that will occur in the pediatric interfaculty transport setting. Through audience participation, we will collect the pertinent clinical information needed to identify the underlying cause of neurologic deterioration. We will then discuss these clinical findings and how they influence decision making when selecting the appropriate therapeutic interventions. The lecture will also review how the recommended guidelines pertain to each patient scenario, formularizing the RT with best practice strategies.
 Neonopolis Entertainment Complex
Neonopolis Entertainment Complex
1:00 pm – 3:15 pm
What You Need to Know About Sleep-disordered Breathing
1:00 pm – 1:30 pm
OSA in the Acutely Hospitalized Patient
Peter C Gay MD, Rochester MN
A discussion of specific conditions associated with OSA in the acute care setting will be followed by a review of the impact of obstructive sleep apnea on treatment and successful patient outcomes.
1:35 pm – 2:05 pm
Sleep-disordered Breathing in CHF
Sairam Parthasarathy MD, Tucson AZ
A discussion of specific conditions associated with congestive heart failure and sleep-disordered breathing will be followed by a review of the impact of SDB on treatment and successful patient outcomes.
2:10 pm – 2:40 pm
Sleep-disordered Breathing in COPD
Peter C Gay MD
A discussion of specific conditions associated with COPD and sleep-disordered breathing will be followed by a review of the impact of SDB on treatment and successful patient outcomes.
2:45 pm – 3:15 pm
Obesity Hypoventilation
Sairam Parthasarathy MD
A discussion of specific conditions associated with obesity hypoventilation will be followed by a review of its impact on treatment and successful patient outcomes.
 Holiday Decorations at the Las Vegas Hilton
Holiday Decorations at the Las Vegas Hilton
1:00 pm – 4:25 pm
Career Development Tune-up
1:00 pm – 1:30 pm
Leadership Gold
Scott Reistad RRT CPFT, Denver CO
There are multiple lessons that leaders learn, some the hard way. In this session, the presenter will help attendees navigate the challenging roles of leading people successfully.
1:35 pm – 2:05 pm
Servant Leadership: Developing the Leader With-in You
Douglas S Laher RRT MBA, Cleveland OH
The best days of the hierarchical leadership model of a top-down approach is behind us, at least hopefully. The value of a servant leader, both to the individuals they support as well as organization, will be described by the presenter, with a highly interactive format to engage the audience.
2:10 pm – 2:40 pm
The Synergy Challenge: Creating the “Win-Win”
Kenneth Thigpen RRT FAARC, Jackson MS
The presenter will “unpack” some unique approaches that are designed to achieve alignment and engagement with work teams. He will provide simple approaches to increase the effectiveness of teams and leaders.
2:45 pm – 3:15 pm
Recruitment and Retention: It’s a Team Effort!
Garry W Kauffman MPA FACHE RRT FAARC, Lancaster PA
For those managers who feel that recruitment, interviewing, orienting, and engaging staff is their job, you are just plain wrong! The presenter will provide a “Top 10” list of how managers and staff must collaborate to get the right respiratory therapist on board and keep them engaged.
3:20 pm – 3:50 pm
Productivity and Benchmarking—Finding the Strength in the Numbers
Richard M Ford RRT FAARC, San Diego CA
The presenter will lead a discussion to address the power of using data to drive and support key decisions. There are significant advantages to dovetail the experiences of others and develope a compelling business case to achieve what is needed to provide exceptional care for our patients and staff.
3:55 pm – 4:25 pm
How Do You Handle: Stump the Experts
Panel Discussion
Attendees will have the opportunity to query the expert panel as to strategies they have implemented in order to handle any one of a myriad of challenges facing leaders and staff today.
 Tom Petty
Tom Petty
1:30 pm – 4:40 pm
Dr. Tom Petty’s Legacy for Respiratory Care
Thomas L Petty, MD FAARC (“Dr. Tom” to thousands of respiratory therapists and patients with lung disease) was one of the true pioneers of our field, with a career spanning half a century. This symposium, held one year after his death, reviews his many major contributions to the understanding and management of pulmonary disease, and celebrates the many ways in which his work and personal charisma have affected both the field and the profession of respiratory care.
1:30 pm – 1:50 pm
Introduction: Who Was Tom Petty?
David J Pierson MD FAARC, Seattle WA
This presentation will give an introductory overview of Dr. Petty’s life, and his contributions both to our knowledge of respiratory illness and to the welfare of patients with lung disease.
1:55 pm – 2:20 pm
Chronic Obstructive Pulmonary Disease and Home Care
Robert W McCoy RRT FAARC, Apple Valley MN
The speaker will present a summary of Dr. Petty’s many important contributions to the development of long-term oxygen therapy, pulmonary rehabilitation, respiratory home care, education of the public, and the early detection of COPD.
2:25 pm – 2:55 pm
The Acute Respiratory Distress Syndrome
David J Pierson MD FAARC
This presentation will summarize and explain Dr. Petty’s role in describing ARDS and establishing the role of PEEP in its management.
3:00 pm – 3:30 pm
Medical Education
Kent Christopher MD RRT FAARC, Denver CO
This presentation reviews Dr. Petty’s seminal contribution as a teacher, not only in training hundreds of clinicians, researchers, and educators in pulmonary medicine (including many of the field’s current leaders worldwide), but also in educating front-line practitioners in his region and internationally, as well as his role as a prolific author and speaker.
3:35 pm – 4:05 pm
The Respiratory Care Profession
Sam P Giordano MBA RRT FAARC, Irving TX
This presentation will highlight Dr. Petty’s long, influential, and sometimes controversial role in promoting respiratory are and advocating for respiratory therapists, including his work with the AARC.
4:10 pm – 4:40 pm
Remembering Tom Petty
Louise M Nett RN RRT FAARC, Denver CO
A personal reminiscence of Dr. Petty as mentor, colleague, and close friend, with reflections on his importance as a pioneer of respiratory care and his legacy for the future.
 Las Vegas Pinball Hall of Fame
Las Vegas Pinball Hall of Fame
2:10 pm – 4:25 pm
The Role of the Respiratory Therapist in Tobacco-dependence Treatment
2:10 pm – 2:40 pm
What Every RT Should Know
Scott Cerreta RRT, Tucson AZ
The speaker will review the “5As” skill and the “AAR” method every RT should know and practice to promote tobacco-dependence treatment, and describe how RTs can complement tobacco-dependence treatment efforts offered through community-based public health organizations.
2:45 pm – 3:15 pm
Integrating Brief Tobacco Interventions into Practice
Jay Taylor AS RRT TTS, Fargo ND
This presentation will describe strategies for integrating tobacco-dependence treatment skills into staff training to empower RTs to become tobacco-dependence treatment advocates, and share helpful hints to enable RT departments to launch a tobacco-dependence treatment program.
3:20 pm – 3:50 pm
Medications for Tobacco-dependence Treatment
Jonathan B Waugh PhD RRT, Birmingham AL
The speaker will describe the array of pharmacological agents currently available to assist with tobacco-dependence treatment efforts and discuss the potential adverse side-effects of certain medications and the appropriate strategy to monitor for such occurrences.
3:55 pm – 4:25 pm
The Stigma of Tobacco and Other Odors in Our Profession
Scott Cerreta RRT
This presentation will describe the direct and indirect effects of lingering tobacco and other offensive odors on the clothing and body of RTs, and discuss how tobacco use among RTs is perceived by other health care workers.
 World’s Largest Chocolate Fountain at Bellagio
World’s Largest Chocolate Fountain at Bellagio
2:30 pm – 4:05 pm
Biomarkers in Exhaled Breath
2:30 pm – 3:15 pm
Clinical Use of Exhaled Nitric Oxide
Michael Davis RRT, Charlottesville VA
Exhaled nitric oxide is a novel non-invasive biomarker with valuable clinical utility to the respiratory therapist. Attendees will be provided with an overview of the history and its role in pulmonary physiology as well as collection methods, case studies, and current research.
3:20 pm – 4:05 pm
Clinical Relevance of Exhaled Breath Condensate pH
John Hunt MD, Charlottesville VA
Airway pH affects both physiologic and cellular lung health. The ability to collect exhaled breath condensate (EBC) provides a non-invasive route for clinicians to measure airway pH. This presentation will discuss the clinical relevance of the acid-base chemistry of the airways and current research.
2:30 pm – 4:30 pm
Vision 2015
The AARC’s 2015 and Beyond project was launched in 2007 to set future directions for the respiratory care profession. The third and final conference took place in July 2010, followed by a Community Input Session aimed at hearing from respiratory therapists across the nation. This presentation will present the final determinations and recommendations.
2:40 pm – 4:05 pm
Around the World
2:40 pm – 3:20 pm
The Agony and Ecstasy of Starting the Respiratory Therapy Profession in a Country of a Billion People
Vijay Deshpande MS RRT, Atlanta GA
and Vijai Kumar R MD DTCD FCCP FAARC, Hyderbad India
Many of the new generation of respiratory therapists in the U.S. are unaware of the challenges faced by early inhalational therapists 40–50 years ago. This presentation will share the experience of starting the respiratory care profession in India with the many challenges that were seen in our country decades ago. Similarities and differences will be shared from personal experiences.
3:25 pm – 4:05 pm
Development of Pediatric Non-invasive Ventilation in Critical Care in Argentina
Gustavo Olguin CRT MHA, Buenos Aires Argentina
Respiratory therapists in the U.S. often take for granted mechanical ventilation protocols and technology. This presentation will share an eye-opening view of the efforts required to develop non-invasive and invasive ventilation programs abroad.
 Open Forum
Open Forum
3:00 pm – 4:55 pm
OPEN FORUMs #12—Asthma/Pulmonary Disease; Aerosols/Drugs
OPEN FORUMs #13—Neonatal/Pediatrics, Part I
Clinicians present the results of their scientific studies. Abstracts with a similar focus are clustered into a symposium to encourage discussions and interactions among investigators and observers; posters expand the information presented. See abstract titles and authors.
3:15 pm – 3:55 pm
Respiratory Care of the Morbidly Obese Patient
John D Davies MA RRT FAARC, Durham NC
Obesity is a public health epidemic affecting the majority of adults. Obesity has a tremendous impact on all organ systems. Respiratory therapists must be armed with the latest research as well as an understanding of anatomy and physiology in order to effectively care for this special patient population.
3:20 pm – 4:10 pm
Pediatric Puzzlers: Stuff You Should See at Least Once
Bruce K Rubin MD MEngr MBA FAARC, Richmond VA
Common practice conditions may present in a very unusual manner. Can you diagnose Dr. Rubin’s clinical dilemmas? Learn from one of the world’s leading pediatric pulmonologists, while having fun at the same time in this interactive session. Is it a horse or a zebra—you decide!
3:20 pm – 5:00 pm
Data in Respiratory Home Care: What We Have—What We Need
3:20 pm – 3:50 pm
Using Medical Device Reporting Data to Improve Home Ventilator Safety
Angela King RPFT RRT-NPS, Detroit MI
Participants will learn how to access the Medical Device Reporting database on the FDA website. The presenter will discuss the most common causes of reported adverse incidents with home mechanical ventilators and strategies to reduce their reoccurrence.
3:55 pm – 4:25 pm
Using a Novel Outcome Survey Tool to Gain Patient Insight
Nicholas J MacMillan AGS RRT FAARC, Stevensville MD
The presenter will discuss the challenges of gathering relevant outcome data in an austre financial environment and will describe a new patient survey instrument and the potential value of and uses for the data obtained.
4:30 pm – 5:00 pm
Collecting and Integrating QI Data for Better Decision Making
Susean L Nichols RRT, Long Beach CA
The presenter will discuss the requisite components of a formal QI program required by all home care accrediting agencies and will provide examples of how data obtained from QI activities can be used to improve day-to-day operations within the organization.
 Hard Rock Casino
Hard Rock Casino
4:00 pm – 5:05 pm
Protocols in Respiratory Care & Demonstrating Value
4:00 pm – 4:30 pm
The Anatomy of a Protocol
Suzan J Herzig RRT, Alpine CA
Thinking about developing protocols? Where do you start? The presenter will work through defining protocols and will outline the building blocks of developing protocols and how to overcome barriers to implementation. Examples of protocols that have been successful and may serve as models for others in developing their programs will be shared.
4:35 pm – 5:05 pm
Protocols—Holding the Gains
Suzan J Herzig RRT
The benefits of protocols will be presented, along with a discussion of how to hold the gains. The process of starting out small, and how to refine and grow your program, will also be discussed. Getting long-term buy-in from staff and physicians is critical and will be reviewed.
4:10 pm – 4:55 pm
Disaster Response—Respiratory Therapists in Action
Michael E Donnellan RRT-NPS MBA, Oakland CA
The speaker will share his experience as a DMAT member and discuss preparations necessary for implementing an adequate response to mass casualty events.
4:20 pm – 5:00 pm
High-Flow Oxygen Therapy: Real Benefit or Just a Fad?
Timothy R Myers RRT-NPS, Cincinnati OH
The use of high-flow oxygen therapy is growing at an exponential rate, but do the available data support this practice? The AARC’s Immediate Past President will review the medical literature and discuss the recent trends in the application of this respiratory support strategy. Is there a real benefit to the use of high-flow oxygen therapy, or is it just a passing fad?
4:30 pm – 5:10 pm
How to Start and Facilitate a Respiratory Care Journal Club
Carl R Hinkson RRT, Seattle WA
This presentation discusses how a journal club for department staff can facilitate professionalism and continuing respiratory care education as well as bolster morale. Included will be practical advice on starting and facilitating a journal club and obtaining CRCE credits as an incentive for staff attendance.
4:35 pm – 5:00 pm
Continuing Care/Rehab Section Membership Meeting
Debra Koehl MS RRT AE-C/Presiding
Section members meet to determine their needs and priorities, as well as how to use the AARC resources to accomplish them. All Congress attendees, including section non-members are invited to attend and to participate.4:35 pm – 5:00 pm
Education Section Membership Meeting
Lynda Goodfellow EdD RRT FAARC/Presiding
Section members meet to determine their needs and priorities, as well as how to use the AARC resources to accomplish them. All Congress attendees, including section non-members are invited to attend and to participate.
